The latest GP appointment stats covering October have led some observers to fanfare that the level of GP appointments is now at pre-pandemic levels. But that conclusion is only partially true, and more fundamentally, perhaps it also misses the point.
It is accurate that the total number of appointments in October was 28.2 million and this is certainly greater than 27.1 million, the figure back in January this year. However, given seasonal fluctuations, it is usually wiser to compare year-on-year figures, and here we see a different story. In October 2020, we were 1.8 million appointments short of the 30 million that were carried out a year ago.
A more fundamental question is whether bigger is always better. This time last year, many were reflecting on whether we could be smarter in the way we manage GP appointments. It is not clear that ever increasing numbers of GP appointments benefits patients, and it certainly places a heavy burden on general practice.
Of course, in a year when there have been 27.5 million fewer GP appointments because of the pandemic compared to this time last year, it seems reasonable to consider volumes as one element of recovery. It just should not be taken as the whole story.
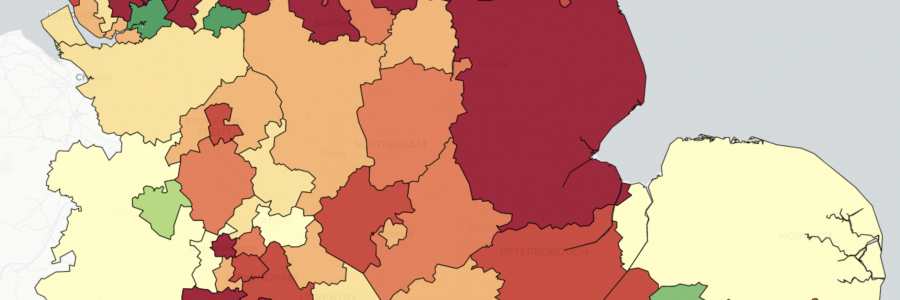
If we look at geographic variation, we see just 16 CCGs where there were more appointments in Oct 2020 than this time last year. Some of the explanation underpinning this may be a wider choice of options, but the considerable geographic variation across the country suggests a more complex picture. The green areas in the map below show where activity has increased year-on-year. Red areas show declines.
Containing the number of patient appointments will only be a good thing if it is done in a sustainable way that supports patients, improving their outcomes and experiences rather than leaving them in the lurch.
While there is clear evidence that some practices are making great strides to provide personalised options for patients, the necessary depth of information is just not available in the currently published data to understand the extent to which we are satisfying patient needs across the board. The DHC will continue to argue strongly for the publication of more meaningful metrics to shed more light on this.
As we look to procure solutions to support GP appointments, we need a rich set of options that allow clinicians to service all patients. We should raise our sights beyond swapping old ways of doing things for alternatives that offer minimal additional benefit. Instead, a joint problem-solving approach is far more likely to lead to genuinely innovative approaches that are necessary to achieve the triple aim: improving patient experience, improving health outcomes, and doing it all much more efficiently.